This guide will help you review Navitus Health Solution’s formulary for your pharmacy benefit.
A formulary helps you understand what medications are covered by your pharmacy benefit and how much you will pay for those medications, as well as special considerations for some medications. The formulary lists medications in several ways:
- The first section lists medications in alphabetical order.
- The second section lists the same medications by class or category.
- The final sections provide more information on medications that require prior authorizations as well as specific lists with additional requirements quantity limits, prior authorization and other special codes.
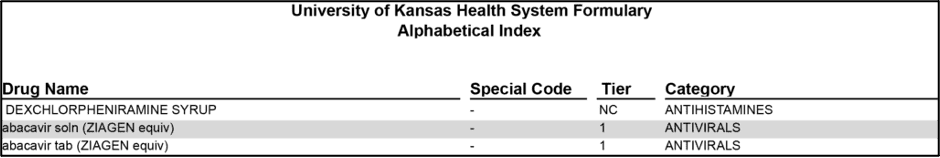
Formulary example
The table pictured here is an example of the formulary’s alphabetical listing of medications.
Formulary definitions
The important definitions below will help you understand the information within each formulary column.
• Drug Name
This column includes the medication name as well as other identifying information. UPPERCASE letters indicate brand-name medications and lowercase letters indicate generic medications.
TIP: It is helpful to know your medication’s active ingredient or brand name. Then you can search the formulary for the medication by clicking the magnifying glass in the PDF toolbar or type CTRL+F to open the “Find” feature.
• Special Code
This column includes letter codes to indicate special considerations for some medications. A key for these letter codes is included at the bottom of every formulary page, but here are definitions for some of the most common codes:
- QL = Quantity Limit drugs are limited in the number of doses you can receive at one time.
- PA = Prior Authorization drugs require additional information from your provider to ensure the medication is right for your situation.
- SF = Split Fill drugs are limited to two 15-day fills per month for the first three months to confirm the medication is right for your situation before filling a larger supply.
- ST = Step Therapy drugs are high-cost medications that may only be prescribed after trying a less costly, clinically equivalent drug first.
- MSP or LD = Mandatory Specialty Pharmacy or Limited Distribution drugs are specialty medications that require special coordination for chronic or complex health conditions.
- RDX = Restricted-to-diagnosis drugs may only be prescribed for a specific medical diagnosis.
- RS = Restricted-to-specialist drugs may only be prescribed by a specialist provider.
For both the Signature Plan and the HSA Advantage Plan, special codes may affect if a prior authorization is needed, where you can fill the prescription and how many days’ supply you can receive. Additionally, special codes – particularly MSP or LD – combined with tiers (defined below) affect Signature Plan copays. Please review the pharmacy benefit charts on our prescription medication coverage page for details. Learn more about copays and coinsurance in our guide to understanding how you and the health system share the cost for your healthcare expenses.
TIP: If your medication has a special code, it is likely also listed in the final pages of the formulary along with important additional information, such as coverage limits or requirements.
• Tier
This column includes number or letter codes to indicate medication cost tiers.
- Tier 1 = Generic medications are the most cost-effective option for many medications. Generic drugs must work in the same way and provide the same clinical benefit as their brand-name counterparts to be approved by the Food and Drug Administration (FDA).
- Tier 2 = Preferred brand medications are brand-name medications that are favored over other brand-name medications on the formulary.
- Tier 3 = Nonpreferred brand medications are the highest cost option for covered medications on the formulary.
- NC = This medication is not covered. You may want to talk with your provider about an alternative medication.
- 50% = 50% coinsurance is required for this medication, regardless of your medical plan.
- OC = This is an oral chemotherapy medication.
Please note that tiers combined with special codes (defined above) – particularly MSP or LD – affect Signature Plan copays. Tiers do not affect HSA Advantage Plan coinsurance percentages but choosing lower-cost generics vs. higher-cost brands can affect HSA Advantage Plan coinsurance amounts. Please review the pharmacy benefit charts on our prescription medication coverage page for details. Learn more about copays and deductible plus coinsurance in our guide to understanding how you and the health system share the cost for your healthcare expenses.
TIP: If you know your medication’s brand name, you can check for a generic equivalent. Click the magnifying glass in the PDF toolbar or type CTRL+F to open the “Find” feature, then type the brand name plus “equiv” in the search bar. The search results will reveal any available generics.
• Category
This column indicates a class or category for each listed medication, such as analgesics, beta-blockers, corticosteroids, diuretics, etc.
TIP: It is helpful to know your condition’s medical name or your medication’s medical action. Then you can search for the condition or action to find similar medications that may have a lower cost.
Please note that the Navitus formulary is subject to change throughout the year. For the most up-to-date information on your prescription medications, login to the Navitus member portal or mobile app.

Use the information on your pharmacy ID card to get started.
