 Pregnancy across all stages
Pregnancy across all stages
Educational resources
The following are excellent resources to guide you and your partner through the pregnancy journey.
- Baby Steps to Motherhood: The Women’s Health experts at The University of Kansas Health System have created a comprehensive digital guidebook to help you have a healthy pregnancy, including information about pregnancy symptoms, health concerns, nutrition, exercise and month-to-month fetal development.
- Free Virtual Childbirth class: Sessions are offered each month by the health system and registration is required. When searching for a class, be sure to change the date range to fit the timeframe you’re looking for.
- Free Virtual Newborn class: If you are expecting or have a new baby, register for the health system’s free virtual newborn class. The class covers common questions about the newborn phase and includes a Q&A with a pediatrician. Sessions are offered each month and registration is required.
- Breastfeeding class: This class will provide you with the essential information you need to get breastfeeding off to a good start.
- CPR Certification Classes: The health system is an authorized training center for the American Heart Association and offers several classes for employees and community members including BLS (basic life support – CPR), ACLS (advanced cardiovascular life support) and PALS (pediatric advanced life support)
- Mayo Clinic Guide to a Healthy Pregnancy, Second Edition by Myra Wick, M.D., Ph.D.
- Obstetricks by Julie Lamppa , APRN, CNM
Health information during pregnancy
Quality prenatal care is important for a happy and healthy pregnancy. During your pregnancy, regularly scheduled appointments with your doctor are important, necessary and covered by your health system medical plan. It is vital to keep each prenatal appointment, so your physician can provide you with important information and monitor your pregnancy progress. This also allows you an opportunity to discuss any concerns or questions you may have as they arise. Prenatal visits are generally scheduled in regular intervals, but if needed the frequency may vary.
Click here for more information about what to expect at prenatal appointments, pregnancy symptoms, pregnancy screenings, recommended vaccines during pregnancy and more.
If at any time during your pregnancy you experience any of the below symptoms, contact your doctor and/or seek medical attention:
· Bleeding or excessive fluid flow from your vagina
· Feeling dizzy or faint
· Shortness of breath
· Chest pain
· Calf pain or swelling
· Painful contractions in uterus
Nutrition
Below are general nutritional guidelines for pregnancy, but be sure to follow your doctor’s advice when it comes to caring for yourself and your baby. To support a baby’s growth, most pregnant individuals need 100 to 300 extra calories per day. Expectant individuals should consume a variety of foods from each of the five food groups each day to provide the nutrients you and your growing baby need. Be aware of your serving sizes during pregnancy – “eating for two” is a common misconception.
- Meals: To help relieve heartburn and discomfort, eat four to six smaller meals each day instead of three big ones.
- Snacks: Eat healthy snacks such as cheese, yogurt, fruit and vegetables. If you’re not allergic, peanut butter and nuts are also a good choice.
- Liquids: Drink at least eight to 10 glasses of water each day. Juice (no more than 6 oz a day) or milk (non-fat or 1% are best) are good choices too.
- Caffeine: Limit your caffeine to 200 milligrams per day, which is about one 12-ounce cup of coffee. The amount of caffeine in one cup of coffee depends on the brand and how it is made, so be sure to check the package label or ask your local coffee shop. You may consider drinking decaffeinated coffee, which has smaller amounts of caffeine. Caffeine can also be found in tea, chocolate, soda and even some over-the-counter medicines.
- Prenatal multivitamins: Take prenatal multivitamins as directed by your doctor.
Eating safely during pregnancy
Food | Recommendations |
Fresh fish | |
Shark, swordfish, king mackerel, tile fish | Do not eat |
Farmed salmon | Eat no more than 1 meal a month |
Albacore tuna (“white” tuna) | Eat no more than 1 meal a week |
Shrimp, canned light tuna, canned or wild salmon, pollock, catfish | Eat no more than 2 meals a week |
Deli meats and smoked fish | |
Deli meat spread | Do not eat |
Hot dogs, lunch meat, deli meat, deli smoked fish | Do not eat unless reheated until steaming hot |
Canned smoked fish or meat spread | Eat no more than 2 meals a week |
Meat – beef, chicken, pork | |
Any meat that is rotten or raw | Do not eat |
Milk and cheese | |
Unpasteurized milk and the following cheeses: feta, brie, Camembert, blue-veined and Mexican-style queso blanco fresco | Do not eat or drink |
Hard cheeses, semi-soft cheeses (like mozzarella), processed cheese slices, cream cheese, cottage cheese, yogurt made with pasteurized milk | Eat all you want |
Skim or 1% pasteurized milk | Drink all you want |
Preventing anemia
- Eat foods rich in iron such as meat, chicken, fish, eggs, dried beans and fortified grains. The form of iron in meat products, called heme, is more easily absorbed than the iron found in vegetables. If you are anemic and you ordinarily eat meat, increasing the amount of meat you consume is the easiest way to increase the iron your body receives.
- Eat foods high in folic acid, such as dried beans, dark green leafy vegetables, wheat germ and orange juice.
- Eat foods high in vitamin C, such as citrus fruits and fresh raw vegetables.
Prenatal exercise

Exercise during pregnancy typically is safe, encouraged and beneficial for both expecting parent and baby, but be sure to talk to your doctor about continuing your pre-pregnancy exercise routine or beginning a new routine during pregnancy. With clearance from their physician, expecting individuals who remain active during pregnancy are more likely to experience:
- Reduced risk of gestational diabetes
- Average shorter time in labor – studies have shown around 50 minutes shorter compared to non-active individuals
- Lower risk of having a cesarean section
- Faster return to pre-pregnancy weight
- Lower risk of postpartum depression
- Better quality of sleep during pregnancy and postpartum
- Overall faster recovery time after giving birth
Expectant individuals who engage in some sort of strength training during pregnancy may experience additional benefits. Strength training during pregnancy can:
- Aid incontinence
- Protect joints (especially your spine)
- Reduce pain and stiffness
- Aid in delivery
- Help prepare you physically for handling your baby, car seat, diaper bag and other baby gear
- Enhance balance and coordination
Babies born to active individuals also have been shown to be born at a healthy birth weight, be better self-soothers throughout the early stages of life and may have an overall higher intelligence level.
Exercising safely
While continuing to exercise or starting a new exercise routine during pregnancy can be intimidating, here are some helpful guidelines to help you be active.
- It is typically safe to continue with your pre-pregnancy exercise routine or begin a new routine during pregnancy, but first consult with your doctor if you have any questions.
- Aerobic and strength exercise are both beneficial during pregnancy. Aim to get 150 minutes of low to moderate intensity activity each week.
- Stay well hydrated during activity to help regulate your heart rate and blood pressure. Signs of dehydration include dizziness, rapid heart rate and dark urine/little urine.
- Be aware of your body temperature and exercise in an environment that allows your body to cool itself. Uncontrolled, elevated core body temperature (such as high fevers, hot water submersion or heat-related illness) can increase risks to you and your baby.
- Invest in supportive clothing, such as supportive bras and belly supports, to wear as needed during exercise.
- Avoid exercises or movements that increase your risk of losing your balance and falling, such as quick lateral movements and long-duration hold yoga poses or stretches. As pregnancy progresses, your center of gravity changes and joints become less stable, which increases your risk of falling.
Remember if at any time during your pregnancy you experience any of the below symptoms, contact your doctor and/or seek medical attention:
- Bleeding or excessive fluid flow from your vagina
- Feeling dizzy or faint
- Shortness of breath prior to beginning exercise
- Chest pain
- Calf pain or swelling
- Painful contractions in uterus
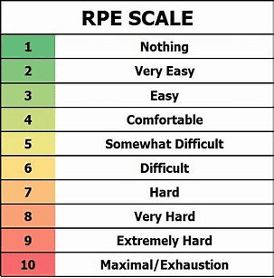
Monitoring exercise intensity
Monitoring the intensity of your workout is critical while exercising during pregnancy. Considering all the physiological changes happening in the body during pregnancy, monitor your exercise intensity using these two effective tests:
- Talk test: You should be able to carry a conversation throughout the duration of your workout.
- RPE scale: Based on the rate of perceived exertion, aim to stay in the light to moderate intensity range most of the time (2- 6). You may venture into vigorous activity/intensity (7-8) for a very short period of time, depending on your physical capacity.
Exercise guidelines
Exercise guidelines
- Always allow for ample time to warm up.
- Focus on training your total body – strengthening your legs, arms, core and back – for your long-term health through pregnancy and beyond.
- Pay attention to special areas of interest that may become “problem” areas during pregnancy, like your lower back, pelvic floor, hips, upper back, abdominals and diaphragm.
- Focus on moving slowly and owning every degree of every exercise – remember what is happening to your musculoskeletal system during pregnancy.
- Abdominal training
- Avoid oblique exercises. Instead, focus on abdominal work that tracks up and down the spine rather than across the body.
- Avoid prolonged time laying on your back, for risk of compressing the vena cava. The vena cava is a large vein that carries blood to your heart from the other areas of the body. If it is compressed due to the weight of the baby and gravity, rolling over and relieving the pressure should eliminate feelings of lightheadedness or numbness.
- When performing abdominal exercises, think about “hugging your baby” or holding your baby high and tight with your abdominal muscles, keeping them engaged throughout your entire workout.
- As pregnancy progresses and your belly grows, performing abdominal exercises may become more challenging but are still important. There are modifications and alternatives to almost every abdominal exercise.
- Pelvic floor strengthening and Kegel exercises
- The pelvic floor undergoes massive changes during and after pregnancy. Being aware of your pelvic floor and how to properly engage it can aid tremendously through all stages of pregnancy and postpartum.
- Doing Kegel exercises is one of the most helpful things you can do to strengthen your pelvic floor and the muscles that support the bladder, uterus and bowels. Daily pelvic floor exercises may help to alleviate or even prevent problems during and after pregnancy, such as incontinence and poor bladder control.
- Low back and lower body training
- Your low back muscles aid in maintaining good posture as your body changes and grows with pregnancy. Engaging your low back muscles will set you up for success as your posture and center of gravity changes throughout pregnancy.
- Exercising your lower back through squats, lunges, wall sits and bridges will strengthen both your lower body and pelvic floor.
- Water-based training
- Engaging in water-based training or activity is a great option during pregnancy, especially the third trimester.
- At all stages of pregnancy, water-based training can allow you to stay active while alleviating many of the discomforts and limitations associated with exercise during pregnancy.
- During water exercise, pregnant women only have to support roughly 50% of their body weight due to the water’s buoyancy. Water eases the pressure on all the joints caused by pregnancy and weight gain, as well as has been shown to relieve chronic low back pain.
Expectations for physical activity during each trimester
Trimester 1
- In your first trimester, many of the noticeable physical changes that come with pregnancy may not yet be relevant. This is a great opportunity to focus on building strength throughout the whole body and becoming familiar with monitoring your exercise intensity.
- Engaging in exercise early in your pregnancy can also aid in managing common first trimester aliments, such as morning sickness and fatigue.
Trimester 2
- As your pregnancy progresses and you begin to notice more physical changes, like your growing belly and breasts, focus on giving yourself proper time to warm up before exercise. Because of the changes in your hormones, your body and joints will need more time to warm up and produce the protective fluid that acts as a cushion between your bones, helping lower your risk of injury during exercise.
- Start learning and practicing correct postural and exercise modifications now, in preparation for your body and the baby’s continued growth.
Trimester 3
- Your third trimester can bring all sorts of discomforts. Movements and workouts you had previously been doing may seem even more challenging.
- As swelling increases, more pressure is placed on your joints, which can result in carpal tunnel. Pregnant individuals will usually experience carpal tunnel of the wrists, causing swelling and numbness in the hands, wrists or even arms. Carpal tunnel typically will subside after the baby is born.
Recommended exercises
Both aerobic conditioning and resistance training are safe and encouraged for most pregnant individuals. You can use these guidelines to develop your own exercise routine.
AEROBIC TRAINING | RESISTANCE TRAINING | ||
Guidelines | Examples | Guidelines | Examples |
· Approx. 150 minutes per week · Two to four sessions per week · Continue until delivery (as tolerated) · Avoid prolonged exposure to heat | · Walking · Running/jogging · Stationary bike/equipment · Prenatal Pilates/yoga · Aquatic exercise | · Two to three sessions per week · Total body workouts · Moderate intensity · Two to four sets of eight to 15 reps per exercise · Practice total core bracing and big, multi-joint movements | · Squats · Hinges · Lunges · Plank variations · Weighted carries · Rows · Pull downs · Overhead presses · Kegels |
Mental health during pregnancy
Pregnancy can be an emotionally sensitive time, marked by changes in hormones, lifestyle, physical health and appearance. Talk to your doctor about how you are feeling and be open and honest with any concerns. If you need additional support:
- Ask your doctor about referring you to a counselor or other professional who can help with anxiety, depression or other mental health struggles.
- Tap into free professional counseling services through our Employee Assistance Program partner, ComPsych. All health system employees, regardless of benefits eligibility, and members of their household have access to eight free confidential counseling sessions per topic.
- For University of Kansas Physicians, The Standard, which is the Employee Assistance Program provider for UKP, offers confidential services and counseling available 24/7. Click here to get started or call 888-293-6948.
- Explore our comprehensive digital Mental Health Resource Guide to access other health system, local and national mental health resources.
Providing support to your pregnant partner
Pregnancy is an emotionally sensitive time for most people, accompanied by changes in lifestyle, physical health and appearances. Partner support is critical to tackling these challenges and has been shown to reduce stress and improve the emotional and physical well-being of the pregnant individuals.
You can be a supportive partner by educating yourself about pregnancy, going with your partner to prenatal care appointments, participating in childbirth classes and joining your partner in making healthy lifestyle choices. The more you learn about what is happening within your partner’s changing body, how it may affect their emotional and physical health and what challenges they may be facing, the better you can support them.
Learn about the development of your baby and how to prepare for childbirth and postpartum, too. These topics should be on your mind as much as your pregnant partner’s mind, and the following resources can help:
- ACOG Partner’s Guide to Pregnancy
- Your Pregnancy and Childbirth: Month to Month
- Mayo Clinic Guide to a Healthy Pregnancy
Open communication is critical to being a supportive partner. Pregnancy can bring up all kinds of emotions, trigger painful memories and unleash strong feelings of self-doubt and fear. Provide your partner with emotional support and be a safe space for them to share whatever is on their mind. If your partner can trust that you’ll listen with an open mind and no topic or concern is off-limits, you’ll be able to provide the emotional support they need.
After the arrival of your baby, consider taking time off work through FMLA, paid time off or other leave of absence to support your partner and family.
Coping with loss
This section includes sensitive information that may be emotionally challenging or triggering for some.
Pregnancy loss
While it is a private topic for most, miscarriage is the most common complication during pregnancy. In fact, at least 15% of all pregnancies end in a miscarriage. There are several signs that can indicate a possible miscarriage. If you notice any of these signs, contact your doctor:
- Abdominal cramping or pain
- Back pain that can range from mild to severe
- Heavy spotting or bleeding
- Vaginal discharge that can include tissue, fluid or blood clots
Although miscarriage is common and does not necessarily indicate an underlying reproductive issue, multiple miscarriages may indicate that further attention is required.
Recurrent pregnancy loss
Recurrent pregnancy loss (RPL) is the miscarriage of two or more consecutive pregnancies that were previously confirmed by a pregnancy test or an ultrasound. There are many possible causes of RPL, including genetics, anatomic issues, immune system, blood clotting, hormonal imbalance and infection. RPL impacts up to 5% of all couples.
The health system offers the TLC program to help individuals and couples navigate RPL. The diagnosis, evaluation and treatment of multiple miscarriages can be an overwhelming process emotionally and physically. The health system’s team of experts will support you through this complex process, providing individualized care and treatment in a supportive environment. Click here to learn about the full range of TLC program services, including egg and sperm donation, fertility evaluation, genetic testing, intrauterine insemination (IUI) and in vitro fertilization (IVF).
Mental health resources to help cope with loss
Coping with and recovering from a loss can be challenging. Talk to your doctor about how you are feeling and be open and honest with your concerns. If you would like additional support, talk to your OBGYN about referring you to a counselor or other professional who can help with anxiety, depression or other mental health struggles.
You also have access to free professional counseling services provided by our Employee Assistance Program partner, ComPsych. All health system employees, regardless of benefits eligibility, and members of their household have access to eight free counseling sessions per topic. Sessions are 100% confidential and available in person, by telephone, via video or through private chat. Click here to get connected.
For University of Kansas Physicians, The Standard, which is the Employee Assistance Program provider for UKP, offers confidential services and counseling as well, available 24/7. Click here to get started or call 888-293-6948.
